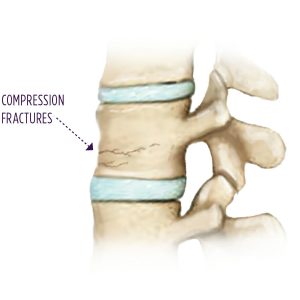
Compression Fractures
Compression fractures are slight breaks that can lead to bone collapses. These compressions often go undiagnosed as patients sometimes assume the pain in their back is the start of arthritis or simply the result of the aging process. If you have even slight pain in your back, you owe it to yourself to visit with our team to determine if there is a compression fracture. Those who are older, and women suffering from weakened bones referred to as osteoporosis, are the most likely to have a compression fracture due to diminished bone density.
The thinning of the bones weakens them to the point that they cannot withstand the pressure and weight of daily activities. It is possible that merely bending forward can lead to a fracturing in the vertebrae that have already weakened. Sadly, two in five women suffer at least one spinal compression fracture by the age of 80. If you have such a compression, obtain medical treatment as soon as possible to decrease the chances of additional compression fractures.
Causes of Compression Fractures
The spine consists of strong segments of bone between the lumbar and cervical portions of the back. The lumbar section is the lower part of the back. The cervical region is the upper part of the back toward the neck. If one or several such bone segments, referred to as vertebrae, collapse, a compression fracture is likely to occur. Such compression fractures within the spine often stem from falls and other injuries.
However, arthritis and osteoporosis that occur as one ages can also lead to compression fractures. It is even possible for a spinal tumor to lead to a compression fracture. Cancer will weaken the supportive bone structures, leading to the destruction of vertebrae, eventually causing a collapse.

Symptoms of Compression Fractures
The symptoms of your compression fracture will likely be somewhat unique to you. The specific pains you feel with such a fracture might not be the exact same as those of another patient. The cause of the compression fracture ultimately shapes the symptoms. However, pain in the lumbar or cervical regions of the back are the most common signs of a compression fracture.
Severe back pain or pain in the back that worsens when walking or standing, are indications of a compression fracture. If you twist or bend and feel pain in your back, become shorter in stature or develop a hunchback, you might have a compression fracture. Pain in the abdominal region is also another common compression fracture symptom. This occurs as the shortened spine pressures the stomach, causing digestive problems such as weight loss, constipation, and loss of appetite. Difficulty when attempting to breathe resulting from spinal compression can lead to lungs that do not function as they should.
Treating a Compression Fracture
Compression fracturs are treated with pain medication, physical therapy that strengthens the back and/or a back brace. Calcium supplements in combination with medications are helpful for patients suffering from osteoporosis. If necessary, surgery will be performed. The kyphoplasty and vertebroplasty procedures are the two most common types of surgeries for compression fractures.
The kyphoplasty is a minimally invasive operations that decreases or completely halts pain resulting from a spinal fracture. The bone is stabilized, and the reduced vertebrae height is restored.
The vertebroplasty procedure is also a minimally invasive surgery that eliminates or reduces the pain stemming from a vertebral fracture. The goal of the vertebroplasty is to provide bone stabilization. A cement that is low viscosity is carefully transmitted into the vertebrae that has collapsed to ensure it is fully stabilized.
We are Accepting New Patients
Our pain management doctors are accepting new patients. To schedule an appointment, please call our Carrollton clinic at (972) 316-7270 or our Denton clinic at (940) 222-8943.

